Metagenics CalmX Technical Information
Metagenics CalmX 10% off RRP at HealthMasters - Click Here
1. META MAG MAGNESIUM, TAURINE AND GLUTAMINE FOR STRESS
Magnesium, taurine and glutamine are key nutrients to reduce the effects of physical and psychological stress on the body. In addition, sufficient amounts of B group vitamins are important for the production of stress-response hormones. Magnesium, in particular, plays a pivotal role in a number of functions in the human body, many of which are brain related. For example, magnesium can reduce the effect of N-methyl-D-aspartate (NMDA) receptor stimulation, by acting as a voltage-gated antagonist at the glutamate NMDA receptor (Figure 1). With chronic stress increasing the hypothalamic NMDA receptor expression, deficiency of magnesium can impact mood with symptoms such as depression, apathy and/or anxiety. Furthermore, studies have demonstrated increased rates of depression in individuals with lower levels of serum zinc; with an inverse relationship seen between lowered zinc status and higher depressive scores. Potassium citrate and glutamine, which enhance the acid-alkaline balance of the body, may also be beneficial for low-grade metabolic acidosis.
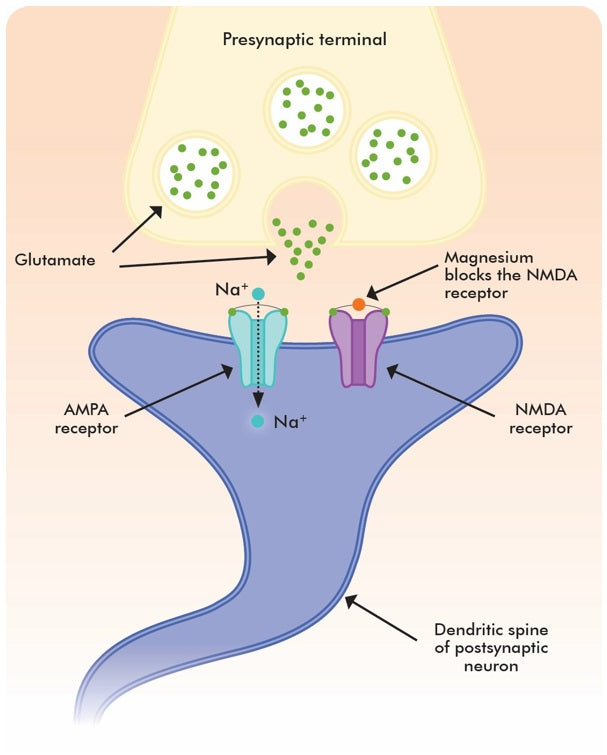
Figure 1: Magnesium reduces the effect of NMDA receptor stimulation by acting as a voltage-gated antagonist at the glutamate NMDA receptor in the brain.
Nutrients That May Assist
- Magnesium - Magnesium amino acid chelate (Meta Mag® - Magnesium bisglycinate)
- Taurine
- Glutamine
- Potassium - Potassium citrate
- Vitamin C - Calcium ascorbate dihydrate
- Vitamin B1 - Thiamine hydrochloride
- Vitamin B2 - Riboflavin sodium phosphate
- Vitamin B3 - Nicotinamide
- Vitamin B5 - Calcium pantothenate
- Vitamin B6 - Pyridoxal 5-phosphate monohydrate
- Zinc - Zinc amino acid chelate (Meta Zn® - Zinc bisglycinate)
Actions
- Nervous system support
- Anxiolytic
- Alkalising
Clinical Applications
- Reduce stress and anxiety
- Supporting healthy mood
Dosing Considerations*
*Dosing regimens should be determined by appropriate assessment and monitoring.
2. BACKGROUND TECHNICAL INFORMATION
Metagenics CalmX 10% off RRP at HealthMasters - Click Here
Magnesium, the Mental Mineral
Magnesium regulates neuronal excitability and membrane fluidity and is arguably the most important micronutrient in relation to nerve and mental function. Magnesium is a cofactor for more than 300 enzymatic reactions in the body1,2 and with many of magnesium’s enzymatic processes being brain-related, deficiency has been associated with a large range of symptoms. These include personality changes such as apathy, depression, confusion, agitation, and delirium.3 Furthermore, low magnesium status has been correlated with other mental health disorders including anxiety,4 psychosis,5 and stress-related conditions such as phobias, tics, obsessive compulsive and dissociative disorders, hyperexcitability, hyper emotivity and other negative emotional states.6
Magnesium deficiency is common, with a recent Australian Health Survey finding 72% of 14-18 year old females, and an average of just under 40% of all Australian adults consuming inadequate amounts of magnesium daily.7 In addition, dietary factors such as high intakes of fat, calcium, coffee and strong tea can worsen magnesium status, by either reducing absorption or enhancing elimination.8
‘Magnesium deficiency has been associated with a large range symptoms and personality changes such as apathy, depression, confusion, agitation and delirium.’
Magnesium Bioavailability
It has been well-established that amino acid chelates offer the best form of delivery for most minerals. Of these, magnesium bisglycinate (Meta Mag) is the most efficient way to present high dose magnesium (regarding absorption and utilisation), due to glycine being the smallest amino acid.9,10 Glycine allows the chelate to be effectively absorbed through amino acid channels for complete utilisation once within the body.11 The combination of minerals with amino acids also mimics the natural delivery of minerals from plant and animal sources,12 therefore delivering them the way they are generally found in nature.
Studies have shown that magnesium bisglycinate is absorbed into enterocytes intact.13 Magnesium then dissociates from glycine within the enterocyte and is delivered rapidly into the blood stream.14 Not only is intestinal uptake (bioavailability) greater with magnesium bisglycinate compared to other forms of magnesium (Figure 2), studies have also shown faster absorption. For example, magnesium bisglycinate was absorbed at a rate 228% higher than that of magnesium chloride in a study carried out on a group of athletic females.15
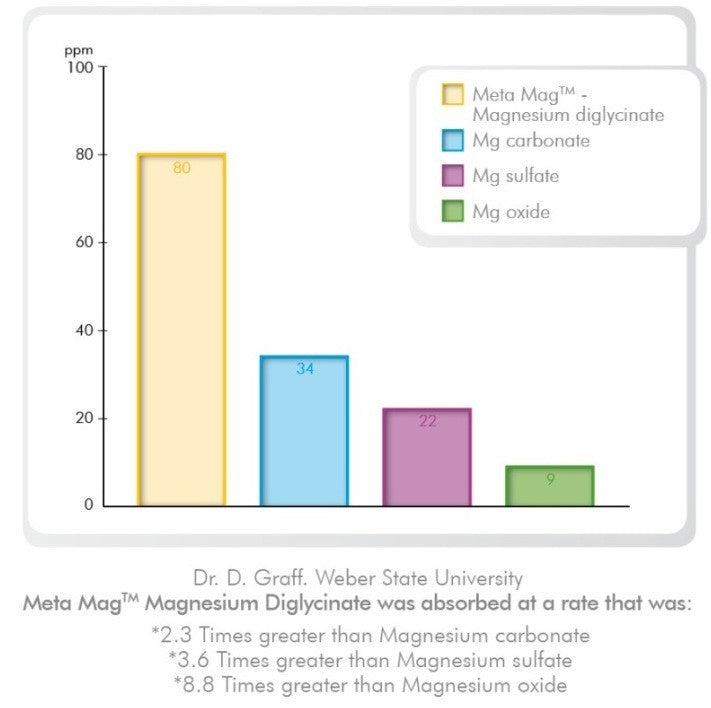
Figure 2: Intestinal uptake rate of different magnesium types.16
3. ACTIONS
Metagenics CalmX 10% off RRP at HealthMasters - Click Here
Nervous System Support
Magnesium supplementation has been shown to affect all elements of the body’s reactions to stress, exerting a neuroprotective effect. For example, in the event of deficiency, magnesium repletion reverses the increased stress sensitivity, with pharmacological loading of magnesium inducing resistance to neuropsychological stressors such as glutamate excitotoxicity.17
Glutamate is an excitatory neurotransmitter important for brain function and development; however, an excess of glutamate can result in neurotoxicity.
With the ability to inhibit the release of excitatory neurotransmitters, magnesium acts as a voltage-gated antagonist at the glutamate, NMDA receptor.18 When the NMDA receptor is over-activated, it can result in increased cell death and increased excitotoxicity which ultimately results in neurological changes. For example, low levels of magnesium has been associated with hippocampal atrophy, with supplementation demonstrating the ability to boost brain derived neurotrophic factor (BDNF) and promote hippocampal neurogenesis.19 Psychological stress is one of the states that can result in the release of glutamate (which exerts excitatory effects), and appears to be mediated, at least in part, via glucocorticoids, which can both increase glutamate levels and contribute to the neuronal damage.20
In a state of deficiency, the neuronal requirements for magnesium may not be met, causing the neuronal damage which can result in low mood.21 Acute stress has been associated with increased plasma magnesium levels due to the release of stress hormones (catecholamines and corticosteroids), and increased urinary excretion.22 This is due to the body shifting magnesium from the intracellular to extracellular space as a protective mechanism to reduce the effects of stress.23 For example, by limiting the rate of inflammation and oxidation experienced at times of stress, as well as supporting extra neurotransmitter requirements.
With extended periods of stress resulting in progressively deficient magnesium levels, a vicious cycle can develop where stress increases cellular magnesium losses, thus resulting in an exaggerated stress response.24 Moreover, magnesium deficiency is itself a stress to the body, as it has been linked to promoting catecholamine release, promoting pro-inflammatory factors, and disrupting sleep patterns.25 Therefore, it is suitable to say that magnesium deficiency is both a cause and a consequence of stress.
The anxiolytic effects of magnesium are similarly attributed to the reduction of glutamate activity, and the increased actions of the gamma aminobutyric acid (GABA)-ergic systems26 (Figure 3). This results in a soothing effect on the entire stress response system,27 as GABA acts as the body’s primary calming influence, working to control and balance the effects of glutamate.
Magnesium ions regulate calcium ions as part of nerve cell conduction activity,28 (Figure 4) with magnesium deficiency causing NMDA-coupled calcium channels to be biased towards opening, leading to further neuronal injury and neurological dysfunction.29 This results in glutamate-induced neuro-excitotoxicity, which may manifest as anxiety and other mood and behavioural disorders.30
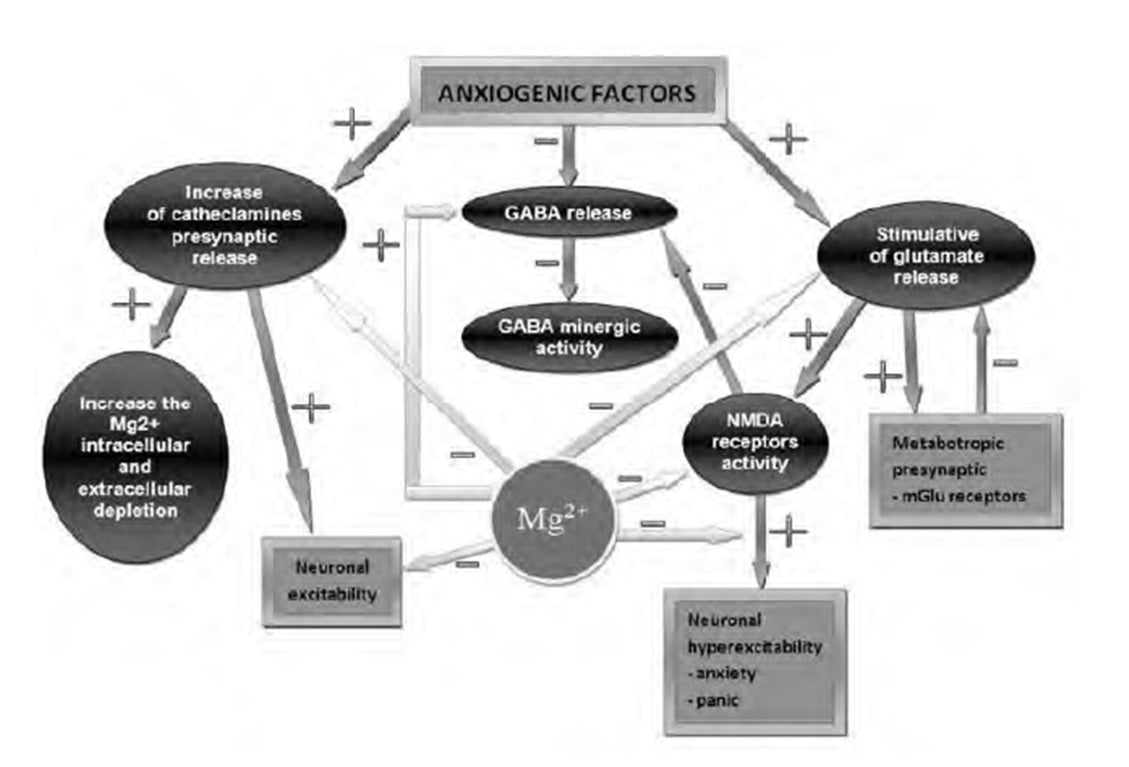
Figure 3: Magnesium’s mechanism of action in anxiety and panic.39
Taurine, (otherwise known as 2-aminoethane sulfonic acid), has modulatory effects on the magnitude of the stress response in the brain. Taurine has been described as a unique psychopharmacological compound,31 which can act as a neuromodulator, an osmoregulator, a regulator of cytoplasmic calcium levels, a neuroprotectant, and a trophic factor in development.32 It is involved in the regulation of calcium movement during depolarisation as well as in maintaining the structural integrity of the neuronal membrane.33 Animal studies indicate taurine exerts anxiolytic34 and antidepressant-like effects, with no alteration of locomotor activity.35
Taurine is found abundantly in the brain.36 It has been shown to act as an inhibitory neurotransmitter or neuromodulator; (thus protecting against glutamate excitotoxicity) and may directly interact at the glutamate NMDA receptor to suppress glutamatergic transmission.37 Furthermore, taurine is reported to be supportive when treating addictions, due to its ability to decrease extracellular basal levels of dopamine as well as prevent acute increases in the synaptic levels of dopamine within the nucleus accumbens;38 the area of the brain involved in reward, motivation and impulsivity.
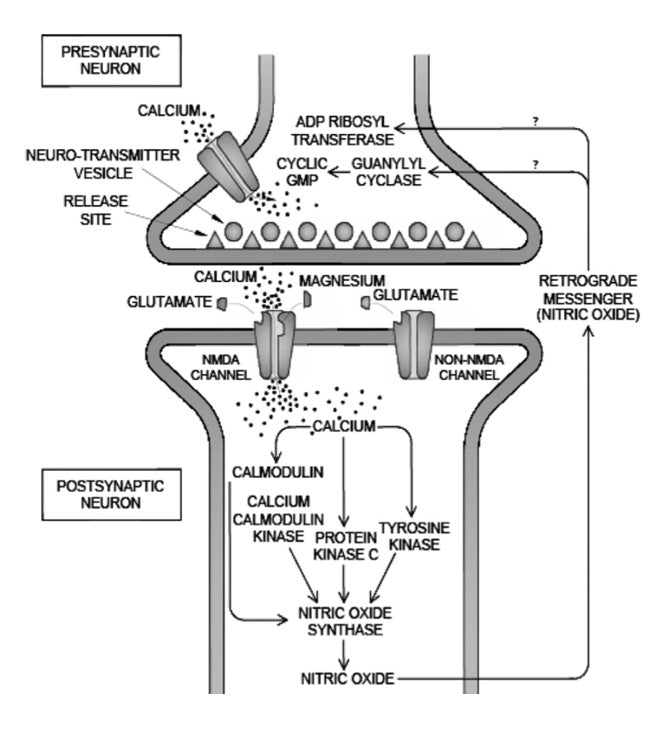
Figure 4: The role of magnesium in regulating calcium ion flow and neurotransmission.40
Zinc is required throughout the human body for a myriad of chemical reactions necessary for normal body functioning.41 For example, it is well-established that zinc supplementation provides antidepressant-like effects, with zinc deficient diets associated with low moods.42 Zinc has been shown to increase BDNF, which is recognised as a target implicated in the aetiology of depression.43 It has been demonstrated that BDNF plays a significant role in supporting patients with low mood, with a meta-analysis showing depressive patients have decreased serum and plasma BDNF levels.44 Zinc is highly concentrated in the synaptic vesicles of specific neurons, and regulates the release of neurotransmitters. The neurons that contain zinc are known as zinc-enriched neurons (ZEN), with cerebellar ZEN primarily associated with GABA neurotransmission, which produces a calming effect by balancing over-excitability. In other regions, ZEN are found in glutamate-producing neurons.45 Furthermore, zinc has been shown to increase synaptic dopamine levels, thereby allowing dopamine to stay and engage with receptors longer within the synapse, and is considered an important regulator of dopamine transporter function.46
Additionally, zinc also acts as an inhibitory neuromodulator of glutamate release, regulating NMDA receptors.47 The areas of the brain in which functional and structural changes occur in the course of low mood are areas of particularly high concentration of glutamatergic neurons sequestering zinc, and the subsequent NMDA receptors are characterised by a high degree of susceptibility to the inhibitory effects of zinc.48 This reflects a further need for sufficient zinc to reduce the excitotoxicity associated with the pathophysiology of mood disorders.
‘It has been well-established that zinc supplementation provides antidepressant-like effects, with zinc deficient diets associated with low moods.’
Moreover, deficiency of thiamine has been associated with decreased glutamate uptake in the brain and increased levels in the cerebrospinal fluid.49 Up to 85% of thiamine content in meat and vegetables is lost with cooking and processing, and there is significant loss with refining of grains.50
L-Glutamine is the most abundant extracellular amino acid and is the precursor for the neurotransmitters glutamate and GABA. It is quantitatively the most important fuel for intestinal tissue, while other functions include its role as a precursor for glutathione production, neurotransmitter synthesis, and its function in controlling acid-base balance.51
Glutathione is the most important intracellular antioxidant, protecting cellular organelles, including the nucleus and DNA, from oxidative damage.
Vitamin C (ascorbic acid) is required for the synthesis of neurotransmitters (including noradrenaline and serotonin), as well as the synthesis and catabolism of tyrosine.52 Vitamin C is maintained at elevated levels in the central nervous system and may act as a neuromodulator, facilitating the release of neurotransmitters and inhibiting glutamate binding to receptors.53 Additionally, the antioxidant properties of vitamin C can assist in reducing reactive oxygen species (ROS), which have been shown to be subsequently increased due to chronic stress.54 The presence of ROS may result in oxidative damage in the central nervous system, which has been demonstrated to play a role in the development of depressive symptoms.
‘Vitamin B6 is a fundamental nutrient for the production of many neurotransmitters.* Deficiency is often associated with psychological disturbances such as mood alterations.’
There are many forms of vitamin C, with calcium ascorbate being the calcium mineral salt of ascorbic acid. This form is buffered and less acidic than ascorbic acid itself. Therefore, it is better tolerated by those who may experience abdominal pain or diarrhoea with ascorbic acid.55
Riboflavin sodium phosphate (vitamin B2, also known as flavin monucleotide or FMN), and its derivative flavin adenine dinucleotide (FAD), functions as a coenzyme for a wide variety of different reactions in intermediary metabolism in the body.56 In particular, riboflavin is involved in the activation of vitamin B6 and folate, which are essential cofactors for the formation and metabolism of neurotransmitters.57 Due to this, it is likely that the production of stress supporting neurotransmitters will be effected without sufficient vitamin B2, resulting in subsequent changes in mood. Regarding nutrient loss in foods; as much as 75% of riboflavin can be lost with cooking.58
Niacin (vitamin B3) is a generic term for nicotinic acid and nicotinamide (niacinamide). Approximately 200 enzymes in the body require, as coenzymes, the nucleotides of niacin: nicotinamide adenine dinucleotide (NADH) and nicotinamide adenine dinucleotide phosphate (NADP). Niacin is therefore important for many biosynthetic pathways. The reduced form of NADH is used for folate metabolism,59 with niacin also able to be converted from tryptophan; a deficiency of niacin can likely impact on the production of serotonin, thereby leading to low mood.60 As much as 75% of niacin in food sources can be lost with cooking.61
‘Magnesium is highly associated with stress levels, with both stress and hypomagnesemia potentiating each other’s negative effects.’
Pantothenic acid (vitamin B5), as part of coenzyme A (CoA) and 4’-phosphopantethiene, participates in nutrient metabolism, resulting in the production of energy and synthetic reactions for the production of many vital compounds within the body. These include bile salts, fatty acids and steroid hormones.62 Vitamin B5’s role in the synthesis of acetylcholine makes it imperative for the ability to cope with stress, with CoA also being required for adrenal cortex function and the synthesis of cortisone.63 Up to 50% of food-derived pantothenic acid can be lost through cooking.64
Pyridoxine (vitamin B6) has many important roles, one of which is in the synthesis of taurine.65 In its coenzyme form, pyridoxal phosphate (PLP), it is associated with over 100 enzymes, the majority of which are involved in amino acid metabolism.66 Vitamin B6 is fundamental to the production of many neurotransmitters67 and is specifically involved in the creation of histidine to histamine, tryptophan to serotonin, glutamate to GABA, and dihydroxyphenylalanine to dopamine,68 as well as the synthesis of adrenaline and noradrenaline.69 Therefore, deficiency in this nutrient is often associated with psychological disturbances such as mood alterations,70 with signs of deficiency including confusion, lethargy and depression. Up to 40% of food-derived vitamin B6 can be lost with cooking.71
Alkalising
Potassium citrate is an effective alkalising agent that can help maintain an optimal pH in the body. pH is a measure of the amount of free hydrogen ions (H+) in a system. The more H+, the lower the pH (i.e. the more acidic a system is). Conversely, the less free H+ (i.e. H+ has been bound to a base pair and is no longer ‘free’) the higher the pH, or the more alkaline a system is; pH 7.0 is considered neutral. The pH of the blood is kept within a narrow range (slightly alkaline, around pH 7.4). There are several mechanisms used to maintain this pH to ensure the body does not become too acidic, including the bicarbonate (HCO3-) buffering system, the phosphate (HPO4) buffering system and the ammonia (NH3) buffering system. Potassium citrate can help to maintain an optimal pH as it dissociates in the body to release citrate that can be metabolised to create HCO-3, which can then be used to balance any excess H+.72,73
The type of diet consumed will affect the buffering mechanisms in the body – both too much acidity or too much alkalinity will make them work harder. Metabolic alkalosis is relatively rare (typically from dehydration, vomiting, or the effects of certain drugs), while metabolic acidosis is much more common. In fact chronic, low grade metabolic acidosis is the norm in Western society.74 The typical Western diet produces a net acid load, which is attributed to the relatively high proportion of acid-forming meats, coupled with acid forming starchy carbohydrates (such as pasta, rice and potato), along with energy-dense, nutrient-poor calories from fats and simple sugars. These are consumed at the expense of alkali-forming foods (fruit and vegetables). Additionally, our high intakes of sodium chloride contribute to this imbalance, placing the body’s metabolic pH buffering system under tremendous strain.
To manage systemic acidosis, diet must be the focus, however supplementation can support the body while dietary changes are being made:
- Glutamine is an important regulator of acid-base balance as it is the most important donor of ammonia in the kidney. Glutamine’s metabolism in the kidney helps to excrete excessive hydrogen ions and maintain blood pH.75 Supplementation with glutamine could potentially spare skeletal muscle from acidosis-induced muscle breakdown.
- Potassium citrate is an effective alkalising agent. Not only is potassium an alkalising agent, citrate is metabolised to bicarbonate in the body, and therefore adds to the buffering potential. Additionally, the citrate anion may be beneficial through its function as an intermediate of the Krebs cycle, with a potential role in energy production.76
4. CLINICAL APPLICATIONS
Metagenics CalmX 10% off RRP at HealthMasters - Click Here
Reduce Stress and Anxiety
Magnesium is highly associated with stress levels, and both stress and hypomagnesemia potentiate each other’s negative effects.77 With extensive reviews performed on magnesium’s association alongside increased stress, Cuciureanu and Vink78 suggest that magnesium should be evaluated in patients presenting with a variety of mental/emotional symptoms, including hyper-emotionality, generalised anxiety, panic attack disorders, insomnia, fatigue and asthenia. They further suggest that alleviation of clinical manifestations with oral supplementation of 5 mg/kg/day can confirm the diagnosis of suspected hypomagnesemia.
In humans, chronic sleep deprivation is associated with progressively decreasing levels of magnesium, with low magnesium being associated with decreased melatonin.79 Additionally, experimental data indicates magnesium deficiency can lead to slightly increased plasma corticosterone levels, increased irritability, aggressive behaviour, disrupted sleep patterns and higher mortality rates in animal studies compared to controls.80
Interestingly, magnesium and oxidative status were investigated in young military volunteers exposed to chronic stress (>10 years) or subchronic stress (>3 months).81 Both of the stress situations caused a significant decrease (p<0.05) in total plasma magnesium, with chronic and subchronic stress causing significant decreases in ionised magnesium compared to the level of ionised magnesium in the control group. The findings of this study supports the need for magnesium supplementation in people living in conditions of stress. Additionally, this study shows that chronic stress of long duration but moderate intensity, as well as subchronic exposure to intense stress, can significantly alter magnesium homeostasis and initiate increased oxidative stress.
Moreover, animal studies of zinc deficiency show increased states of aggression and anxiety, with anxiety-like behaviours shown to develop within just two weeks of being fed a zinc deficient diet.82 The animal models of zinc deficiency have also demonstrated a lowered stress response, with lower zinc levels correlating to higher corticosterone levels following stress in comparison to controls, suggesting zinc to be an important factor in both the modulation of anxiety and stress responses.
Additionally, taurine was found to exert an anxiolytic-like effect in animal models of anxiety.83 Taurine was administered 30 min before the stress tests, and was demonstrated to have significant anxiolytic-like effects by acting as an anti-anxiety agent in the central nervous system.84
Supporting Healthy Mood
A recent review of magnesium for treatment-resistant depression reveals a long history of magnesium being used for low mood. For example, almost 100 years ago, patients with agitated depression were given magnesium hypodermically, with 220 out of 250 doses causing patients to relax and sleep for four to six hours.85 More recently, intravenous and oral magnesium protocols have been reported to rapidly ameliorate major depression safely, and without side-effects.86
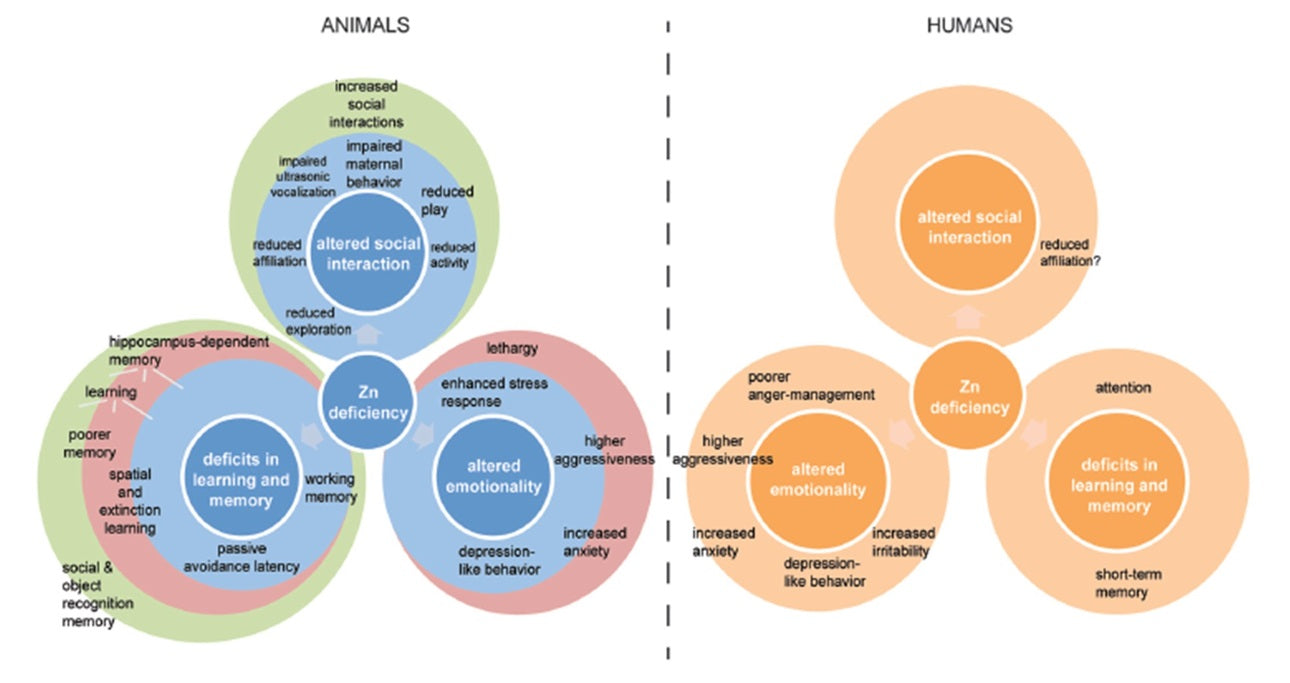
Figure 5: Behavioural alterations reportedly associated with zinc deficiency in animals and humans.87
Decreased magnesium intake has been strongly associated with depression in a study consisting of over 5700 community-dwelling middle-age and older adults, even after adjustments for age, gender, body type, blood pressure, socioeconomic and lifestyle factors.88 In a randomised trial of elderly subjects with type 2 diabetes and hypomagnesaemia (low serum magnesium), magnesium was shown to be as effective as a tricyclic antidepressant (TCA) in the treatment of low mood.89 The elderly participants were given a solution with the equivalent of 450 mg elemental magnesium or the TCA (imipramine) daily for 12 weeks. The results presented significantly improved symptoms of depression, with no significant difference in the mood scores between the groups, demonstrating the magnesium to be as effective as the TCA.
Additionally, magnesium and vitamin B6 have both been demonstrated to be beneficial for improving premenstrual mood of women, in isolation90,91 or combination.92 Fourty-four women (average age 32) were randomly assigned to take consecutively: 200 mg magnesium (as oxide), 50 mg vitamin B6, a combination of the magnesium and B6, or placebo for one menstrual cycle. The results showed a significant effect of the combination of 200 mg/day magnesium with 50 mg/day vitamin B6 on reducing anxiety-related premenstrual symptoms (nervous tension, mood swings, irritability, or anxiety) demonstrating that the synergistic effects of the nutrients were greater than the effect of the magnesium or B6 in isolation.93
Interestingly, zinc has been associated with numerous behavioural alterations in both humans and animals (Figure 5).94 Notably, serum zinc levels have been correlated with severity of depression, with zinc supplementation used in the augmentation therapies as a treatment for depression.95 It has been confirmed in multiple studies that the more severe the depressive symptoms in patients, the lower the serum zinc, compared to non-depressed controls.96
For example, in a study investigating serum levels of zinc in unipolar depressed subjects, patients with minor depression displayed serum zinc levels approximately 93% that of the control group, whereas patients with major depression had serum zinc levels approximately 88% compared to controls (p<0.001).97 Moreover, in a study of 100 adolescent female students with mood disorders, decreased serum zinc was shown to be inversely correlated with the presenting symptoms of depression and anxiety.98 The subjects were assessed for serum zinc levels, with each 10 µg/dL increment in serum zinc levels leading to 0.3 and 0.01 decrease in depression and anxiety scores respectively (p<0.05). The results indicated that the higher the depression and anxiety scores, the lower the patient’s serum zinc, suggesting zinc may be an important supporting nutrient for patients with (or at risk of) mood disorders.
Furthermore, zinc supplementation has been shown to be an effective adjuvant agent in the management of patients with schizophrenia, alongside the anti-psychotic rispiridone. Thirty inpatients with schizophrenia were randomly allocated to receive rispiridone (6 mg/day) plus zinc sulphate (50 mg elemental zinc) three times per day, or respiridone (6 mg/day) plus placebo. Psychotic symptoms and aggression scores were assessed, with the results displaying significantly greater improvements over six weeks in the group receiving zinc sulphate alongside rispiridone, compared to the group receiving placebo alongside rispiridone (Figure 6).99 The results of this study further confirm the beneficial effects of zinc for the potentially profound mood regulatory activity.
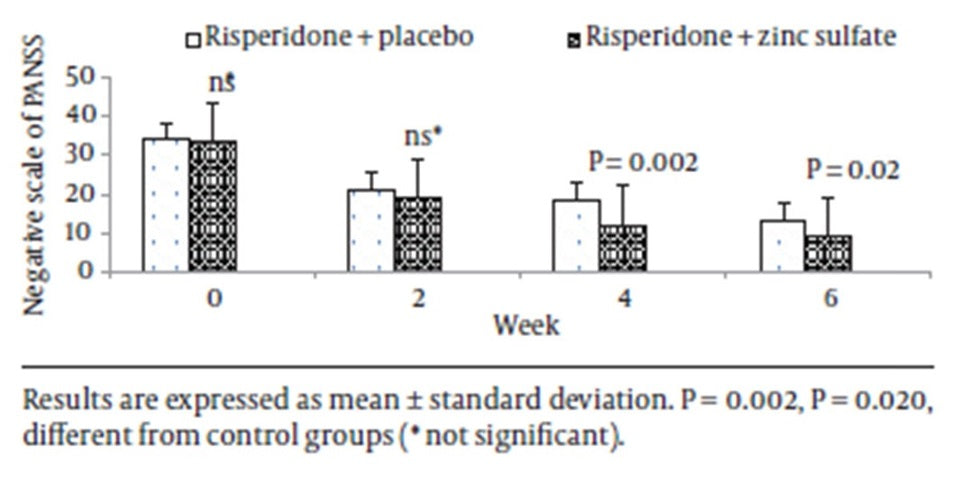
Figure 6: The reduction of negative symptoms in patients with schizophrenia with the combination of rispiridone plus zinc.100
Additionally, thiamine and vitamin C have also demonstrated therapeutic potential in the treatment of low mood. For example, in a 12 week randomised double-blind placebocontrolled trial of patients with major depressive disorder (MDD), the combination of thiamine with antidepressant medication resulted in faster improvement of symptoms. Fiftyone inpatients with MDD were prescribed the selective serotonin reuptake inhibitor (SSRI) fluoxetine (20 mg/day), and randomised to receive either thiamine (300 mg/day) or placebo. After six weeks, the remission rates were greater for the patients receiving thiamine compared to placebo (p=0.001) with all patients reaching a similar remission rate after 12 weeks. The results of the study indicate that the adjuvant administration of thiamine accelerated the improvement in depressive symptoms in patients taking the SSRI, compared to patients taking placebo with the SSRI. Furthermore, in an animal model of depression, vitamin C was shown to improve mood as effectively as fluoxetine,101 indicating the potential beneficial effects of vitamin C to support states of low mood in patients.
5. CAUTIONS AND CONTRAINDICATIONS
Metagenics CalmX 10% off RRP at HealthMasters - Click Here
Contraindications
- Hepatic disease; including liver cirrhosis, hepatic encephalopathy and other severe hepatic disorders: Glutamine, which is metabolised to ammonia, may lead to accumulation of nitrogen/ammonia waste in the blood increasing the risk of ammonia-based encephalopathy and coma. Avoid use. 102,103
- Chronic renal failure: Glutamine should be used under medical supervision in people with chronic renal failure.104,105
- Anticonvulsants/antiepileptic drugs: Glutamine, which is metabolised to the excitatory neurotransmitter glutamate, might antagonise the anticonvulsant effects of medications taken for epilepsy and increase the risk of seizures in some patients. There have been anecdotal reports of such adverse effects. Use with caution and monitor patient symptoms.106 Drugs include, but are not limited to, Carbamazepine, Phenobarbital, Phenytoin, Primidone and Valproate.
- Chemotherapy/Radiotherapy: It has generally been thought that antioxidants may interfere with chemotherapy and/or radiotherapy by decreasing the efficacy of the treatment, but recent studies have found that antioxidants are safe to use in conjunction with these treatments. However, it is still advisable to check with a patient’s oncologist before recommending a formula containing antioxidants.107,108
- Epilepsy and seizure disorders: Excess amounts of glutamine and its metabolite, glutamate, might lower the seizure threshold.109 Avoid glutamine use in these patients. </ul>
- Phenobarbital:
- Phenytoin:
- Allergies and sensitivities:
- Amiloride: Amiloride has been reported to reduce zinc excretion leading to zinc accumulation. Monitor zinc status.116,117
- Amiodarone: Conflicting information exists regarding potential interactions between amiodarone and pyridoxine. Case reports suggest that pyridoxine could exacerbate amiodarone-induced photosensitivity. Mechanisms for this effect are unknown. Monitor patient for signs of photosensitivity.118,11
- Antibiotics: Magnesium and zinc may form insoluble complexes with some antibiotics. Separate doses by at least 2 hours.120,121,122,123
- Bipolar disorder: Glutamine is a precursor of the excitatory neurotransmitter glutamate which can cause affective changes in people with mania or hypomania. There have been anecdotal reports of such adverse effects. Use with caution and monitor patient symptoms.124,125
- Bisphosphonates: Magnesium may form insoluble complexes with bisphosphonates. Separate doses by at least 2 hours.126
- Gout: Large doses of niacin or nicotinamide may impair uric acid excretion and worsen hyperuricaemia in patients with gout. Monitor symptoms and uric acid levels in patients with a history of gout if doses approach this level.127,128
- Haemochromatosis and other diseases of iron accumulation: Vitamin C increases iron absorption; use with caution in cases of uncontrolled haemochromatosis, thalassaemia, sideroblastic anaemia or erythrocyte glucose-6-phosphate dehydrogenase deficiency.129,130 Consider using iron studies to monitor patient iron levels in these patients.
- Hypertension/antihypertensive medication: Preliminary clinical evidence suggests that taking taurine reduces both systolic and diastolic blood. Taurine may have additive effects when used in combination with antihypertensive drugs and may increase the risk of blood pressure becoming too low. Use with caution and monitor blood pressure.131
- Lithium: Taurine can potentially interact with lithium.132 Theoretically, taurine may reduce the excretion of lithium. Taurine is thought to have diuretic properties which might reduce excretion and increase levels of lithium. The dose of lithium might need to be altered and use should be supervised by the pharmaceutical prescriber.133
- Insulin and other hypoglycaemic medications: Niacin and nicotinamide can interfere with blood glucose control requiring dosing adjustment of antidiabetic agents. May cause hyperglycaemia, abnormal glucose tolerance, and glycosuria in diabetic patients.134 In nondiabetic patients, changes in blood glucose are generally small and levels remain within the normal range. About 10% to 35% of diabetic patients may need adjustments in hypoglycaemic therapy when niacin/nicotinamide is added to their regime. Monitor symptoms in diabetic patients.135
- NSAIDs: Zinc may form insoluble complexes with certain NSAIDs. Separate doses by at least 2 hours.136,137
- Safe to use in pregnancy and breastfeeding.
- 1 Hendler SS, Rorvik D (editors). Magnesium. In: PDR for Nutritional Supplements, 1st ed. Montvale: Thomson PDR. 2001:288-295.
- 2 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 3 Serefko A, Szopa A, Poleszak E. Magnesium and depression. Magnes Res. 2016;29(3):112-119.
- 4 Boyle NB, Lawton CL, Dye L. The effects of magnesium supplementation on subjective anxiety. Magnes Res. 2016;29(3):120-125.
- 5 Nechifor M. Magnesium in psychoses (schizophrenia and bipolar disorders). In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:313-330.
- 6 Papadopopol V, Nechifor M. Magnesium in neuroses and neuroticism. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:269-281.
- 7 Australian Bureau of Statistics (ABS). Australian Health Survey: Usual Nutrient Intakes 2011-12. [Online]. 2015. Available from: www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.008~2011-12~Main%20Features~Magnesium~406. [Cited 13/01/17].
- 8 Serefko A, Szopa A, Poleszak E. Magnesium and depression. Magnes Res. 2016;29(3):112-119.
- 9 Siebrecht S. Magnesium bisglycinate as safe form for mineral supplementation in human nutrition. International Journal of Orthomolecular and Related Medicine. 2013:144.
- 10 Albion Human Nutrition. Why Chelated Minerals are Not Created Equal. [Online]. 2016. Available from: www.albionnutritionalfacts.com/index.php/knowledgebase/about-knowledge-base/33-knowledge-base/about-chelated-minerals/60-why-chelated-minerals-are-not-created-equal?start=1. [Cited 17/01/17].
- 11 Siebrecht S. Magnesium bisglycinate as safe form for mineral supplementation in human nutrition. International Journal of Orthomolecular and Related Medicine. 2013:144.
- 12 Siebrecht S. Magnesium bisglycinate as safe form for mineral supplementation in human nutrition. International Journal of Orthomolecular and Related Medicine. 2013:144.
- 13 Schuette SA, Lashner BA, Janghorbani M. Bioavailability of magnesium diglycinate vs magnesium oxide in patients with ileal resection. J Parenter Enteral Nutr. 1994 Sep-Oct;18(5):430-435.
- 14 Siebrecht S. Magnesium bisglycinate as safe form for mineral supplementation in human nutrition. International Journal of Orthomolecular and Related Medicine. 2013:144.
- 15 Albion® Research Notes. 2003 Oct;12(3):2-3.
- 16 Graff D. Bioavailability of magnesium chelazome®Albion® Research Notes. 2000 Mar;9(1):2-3.
- 17 Galland L. Magnesium, stress and neuropsychiatric disorders. Magnes Trace Elem. 1991-1992;10(2-4):287-301.
- 18 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 19 Abumaria N, Yin B, Zhang L, et al. Effects of elevation of brain magnesium on fear conditioning, fear extinction, and synaptic plasticity in the infralimbic prefrontal cortex and lateral amygdala. J Neurosci. 2011 Oct;31(42):14871-14881.
- 20 Smith MA. Hippocampal vulnerability to stress and aging: possible role of neurotrophic factors. Behav Brain Res. 1996;78(1):25-36.
- 21 Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
- 22 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 23 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 24 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 25 Vink R. Magnesium and neurology: new applications for an old friend. Metagenics Congress. June 2016.
- 26 Papadopopol V, Nechifor M. Magnesium in neuroses and neuroticism. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:269-281.
- 27 Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
- 28 Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
- 29 Eby GA, Eby KL. Magnesium for treatment-resistant depression: A review and hypothesis. Medical Hypotheses. 2009;74:649-660.
- 30 Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
- 31 Banerjee SP, Ragnauth A, Chan CY, et al. Neuropsychopharmacological Actions of Taurine. In: El Idrissi AE, L’Amoreaux WJ. Taurine 8. Adv Exp Med Bio. 2013;775:3-18.
- 32 Kuman N, Prentic H, Wu JY. Taurine and its neuroprotective role. In: El Idrissi AE, L’Amoreaux WJ. Taurine 8. Adv Exp Med Bio. 2013;775:19-27.
- 33 Zhang CG, Kim S. Taurine induces anti-anxiety by activating strychnine-sensitive glycine receptor in vivo. Ann Nutr Metab. 2007;51(4):379-386.
- 34 Mezzomo NJ, Silveira A, Giuliani GS, et al. The role of anxiety-life behaviors in zebrafish: A comparative study using the novel tank and the light-dark tasks. Neurosci Lett. 2016 Feb;613:19-24.
- 35 Kong WX, Chen SW, Li YL, et al. Effects of taurine on rat behaviors in three anxiety models. Pharmacol Biochem Behav. 2006;83(2):271-276.
- 36 Leon R, Wu H, Jin Y, et al. Protective function of taurine in glutamate-induced apoptosis in cultured neurons. J Neurosci Res. 2009 Apr;87(5):1185-1194.
- 37 El Idrissi A, Trenkner E. Taurine as a modulator of excitatory and inhibitory neurotransmission. Neurochem Res. 2004;29(1):189-197.
- 38 Banerjee SP, Ragnauth A, Chan CY, et al. Neuropsychopharmacological Actions of Taurine. In: El Idrissi AE, L’Amoreaux WJ. Taurine 8. Adv Exp Med Bio. 2013;775:3-18.
- 39 Papadopopol V, Nechifor M. Magnesium in neuroses and neuroticism. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:269-281.
- 40 Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Medical Hypotheses. 2006;67:366.
- 41 Braun L, Cohen M. Riboflavin. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1197-1223.
- 42 Manosso LM, Moretti M, Ribeiro CM, et al. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
- 43 Manosso LM, Moretti M, Ribeiro CM, et al. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
- 44 Manosso LM, Moretti M, Ribeiro CM, et al. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
- 45 Braun L, Cohen M. Zinc. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1197-1223.
- 46 Braun L, Cohen M. Zinc. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1202-1213.
- 47 Gower-Winter SD, Levenson CW. Zinc in the central nervous system: From molecules to behavior. BioFactors. 2012;38(3):186-193.
- 48 Siwek M, Sowa-Kucma M, Styczen K, et al. Decreased serum zinc concentration during depressive episode in patients with bipolar disorder. J Affect Dis. 2016 Jan;190:272-277.
- 49 Carvalho FM, Pereira SR, Pires RG, et al. Thiamine deficiency decreases glutamate uptake in the prefrontal cortex and impairs spatial memory performance in a water maze test. Pharmacol Biochem Behav. 2006 Apr;83(4):481-489.
- 50 Braun L, Cohen M. Vitamin B1. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1052.
- 51 Newsholme P, Procopio J, Lima MM, et al. Glutamine and glutamate--their central role in cell metabolism and function. Cell Biochem Func. 2003;21(1):1-9.
- 52 Gropper SS, Smith JL, Groff JL. Vitamin C. In: Advanced nutrition and human metabolism. 4th ed. Belmont, CA: Thomson Wadsworth. 2005:260-275.
- 53 Moretti M, Colla A, de Oliveira Balen G, et al. Ascorbic acid treatment, similarly to fluoxetine, reverses depressive-like behavior and brain oxidative damage induced by chronic unpredictable stress. J Psychiatr Res. 2012 Mar;46(3):331-340.
- 54 Moretti M, Colla A, de Oliveira Balen G, et al. Ascorbic acid treatment, similarly to fluoxetine, reverses depressive-like behavior and brain oxidative damage induced by chronic unpredictable stress. J Psychiatr Res. 2012 Mar;46(3):331-340.
- 55 The Linus Pauling Institute. Vitamin C Supplemental Forms. [Online]. 2016. Available from: http://lpi.oregonstate.edu/mic/vitamins/vitamin-C/supplementalforms. [Cited 24/01/17].
- 56 Gropper SS, Smith JL, Groff JL. Vitamin B2. In: Advanced nutrition and human metabolism. 4th ed. Belmont, CA: Thomson Wadsworth. 2005:281-286.
- 57 Braun L, Cohen M. Vitamin B2. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1064.
- 58 Braun L, Cohen M. Vitamin B2. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1063.
- 59 Gropper SS, Smith JL, Groff JL. Vitamin B3. In: Advanced nutrition and human metabolism. 4th ed. Belmont, CA: Thomson Wadsworth. 2005:286-291.
- 60 Braun L, Cohen M. Vitamin B3. In: Herbs and natural supplements: an evidence-based guide. 3rd ed. Sydney: Elsevier/Churchill Livingstone. 2010:938.
- 61 Braun L, Cohen M. Vitamin B3. In: Herbs and natural supplements: an evidence-based guide. 3rd ed. Sydney: Elsevier/Churchill Livingstone. 2010:937.
- 62 Gropper SS, Smith JL, Groff JL. Vitamin B5. In: Advanced nutrition and human metabolism. 4th ed. Belmont, CA: Thomson Wadsworth. 2005:291-295.
- 63 Braun L, Cohen M. Vitamin B5. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1072.
- 64 Braun L, Cohen M. Vitamin B5. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1071.
- 65 Gropper SS, Smith JL, Groff JL. Vitamin B6. In: Advanced nutrition and human metabolism. 4th ed. Belmont, CA: Thomson Wadsworth. 2005:319.
- 66 Braun L, Cohen M. Vitamin B6. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1079.
- 67 Gropper SS, Smith JL, Groff JL. Vitamin B6. In: Advanced nutrition and human metabolism. Belmont, CA: Thomson Wadsworth. 2005:316-321.
- 68 Gropper SS, Smith JL, Groff JL. Vitamin B6. In: Advanced nutrition and human metabolism. Belmont, CA: Thomson Wadsworth. 2005:316-321.
- 69 Braun L, Cohen M. Vitamin B6. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1079.
- 70 Braun L, Cohen M. Vitamin B6. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1079.
- 71 Braun L, Cohen M. Vitamin B6. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2007:1079.
- 72 Frassetto LA, Morris RC Jr, Sellmeyer DE, et al. Adverse effects of sodium chloride on bone in the aging human population resulting from habitual consumption of typical American diets. J Nutr. 2008 Feb;138(2):419S-422S.
- 73 Minich DM, Bland JS. Acid-alkaline balance: role in chronic disease and detoxification. Altern Ther Health Med. 2007 Jul-Aug;13(4):62-65.
- 74 Sebastian A, Harris ST, Ottaway JH, et al. Improved mineral balance and skeletal metabolism in postmenopausal women treated with potassium bicarbonate. N Engl J Med. 1994 Jun;330(25):1776-1781.
- 75 Newsholme P, Procopio J, Lima MM, et al. Glutamine and glutamate - their central role in cell metabolism and function. Cell Biochem Funct. 2003;21(1):1-9.
- 76 Minich DM, Bland JS. Acid-alkaline balance: role in chronic disease and detoxification. Altern Ther Health Med. 2007 Jul-Aug;13(4):62-65.
- 77 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 78 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 79 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 80 Cuciureanu MD, Vink R. Magnesium and Stress. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:251-268.
- 81 Cernak I, Savid V, Kotur J, et al. Alterations in magnesium and oxidative status during chronic emotional stress. Magnes Res. 2000 Mar;13(1):29-36.
- 82 Cope EC, Levenson CW. Role of zinc in the development and treatment of mood disorders. Curr Opin Clin Nutr Metab Care. 2010 Nov;13(6):685-689.
- 83 Kong WX, Chen SW, Li YL, et al. Effects of taurine on rat behaviors in three anxiety models. Pharmacol Biochem Behav. 2006;83(2):271-276.
- 84 Kong WX, Chen SW, Li YL, et al. Effects of taurine on rat behaviors in three anxiety models. Pharmacol Biochem Behav. 2006;83(2):271-276.
- 85 Eby GA, Eby KL. Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses. 2010;74(4):649-660.
- 86 Eby GA, Eby KL, Murck H. Magnesium and major depression. In: Vink R, Nechifor M. Magnesium in the Central Nervous System. Adelaide: University of Adelaide Press. 2011:313-330.
- 87 Hagmeyer S, Haderspeck JC, Grabrucker AM. Behavioral impairments in animal models for zinc deficiency. Front Behav Neurosci. 2015 Jan;8:443.
- 88 Jacka, FN, Overland S, Stewart R, et al. Association between magnesium intake and depression and anxiety in community-dwelling adults: the Hordaland health Study. Australasian Psychiatry. 2009;43(1):45-52.
- 89 Barragan-Rodriguez L, Rodriguez-Moran M, Guerrero-Romero F. Magnes Res. Efficacy and safety of oral magnesium supplementation in the treatment of depression in the elderly with type 2 diabetes: a randomized, equivalent trial. 2008 Dec;21(4):218-223.
- 90 Doll H, Brown S, Thurston A, et al. Pyridoxine (vitamin B6) and the premenstrual syndrome: a randomized crossover trial. J R Coll Gen Pract. 1989;39(326):364-368.
- 91 Facchinetti F, Borella P, Sances G, et al. Oral magnesium successfully relieves premenstrual mood changes. Obstet Gynecol. 1991 Aug;78(2):177-181.
- 92 De Souza MC, Walker AF, Robinson PA. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000 Mar;9(2):131-139.
- 93 De Souza MC, Walker AF, Robinson PA, et al. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000 Mar;9(2):131-139.
- 94 Hagmeyer S, Haderspeck JC, Grabrucker AM. Behavioral impairments in animal models for zinc deficiency. Front Behav Neurosci. 2015 Jan;8:443.
- 95 Manosso LM, Moretti M, Ribeiro CM, et al. Antidepressant-like effect of zinc is dependent on signaling pathways implicated in BDNF modulation. Prog Neuropsychopharmacol Biol Psychiatry. 2015 Jun;59:59-67.
- 96 Cope EC, Levenson CW. Role of zinc in the development and treatment of mood disorders. Curr Opin Clin Nutr Metab Care. 2010 Nov;13(6):685-689.
- 97 Maes M, D’Haese PC, Scharpe S, et al. Hypozincemia in depression. J Affect Disord. 1994 Jun;31(2):135-140.
- 98 Tahmasebi K, Amani R, Nazari Z, et al. Association of mood disorders with serum zinc concentrations in adolescent female students. Biol Trace Elem Res. 2017 Jan;[Epub ahead of print].
- 99 Mortazavi M, Farzin D, Zarhghami M, et al. Efficacy of zinc sulfate as an add-on therapy to risperidone versus risperidone alone in patients with schizophrenia: a double-blind rendomised placbo-controlled trial. Iran J Psychiatry Behav Sci. 2015 Sep;9(3):853.
- 100 Mortazavi M, Farzin D, Zarhghami M, et al. Efficacy of zinc sulfate as an add-on therapy to risperidone versus risperidone alone in patients with schizophrenia: a double-blind rendomised placbo-controlled trial. Iran J Psychiatry Behav Sci. 2015 Sep;9(3):853.
- 101 Moretti M, Colla A, de Oliveira Balen G, et al. Ascorbic acid treatment, similarly to fluoxetine, reverses depressive-like behavior and brain oxidative damage induced by chronic unpredictable stress. J Psychiatr Res. 2012 Mar;46(3):331-340.
- 102 Braun L, Cohen M. Glutamine. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:640.
- 103 Natural Medicines. Glutamine. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=878. [Cited 16/01/17].
- 104 Braun L, Cohen M. Glutamine. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:640.
- 105 University of Maryland Medical Center. Glutamine. [Online]. 2015. Available from: http://umm.edu/health/medical/altmed/supplement/glutamine. [Cited 1/02/2017].
- 106 Natural Medicines. Glutamine. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=878. [Cited 16/01/17].
- 107 Simone CB 2nd, Simone NL, Simone V, et al. Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, part 1. Altern Ther Health Med. 2007 Jan-Feb;13(1):22-28.
- 108 Simone CB 2nd, Simone NL, Simone V, et al. Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, part 2. Altern Ther Health Med. 2007 Jan-Feb;13(1):28-39.
- 109 Natural Medicines. Glutamine. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=878. [Cited 16/01/17].
- 110 Natural Medicines. Glutamine. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=878#scientificName. [Cited 1/02/17].
- 111 Braun L, Cohen M. Vitamin B6. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1088.
- 112 Natural Medicines. Glutamine. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=878#scientificName. [Cited 1/02/17].
- 113 Braun L, Cohen M. Vitamin B6. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2010:1088.
- 114 Natural Medicines. Glutamine. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=878. [Cited 16/01/17].
- 115 Natural Medicines. Niacin. [Online]. 2017. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=924. [Cited 16/01/17].
- 116 Braun L, Cohen M. Zinc. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1219.
- 117 Natural Medicines. Zinc. [Online]. 2017. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=982. [Cited 16/01/17].
- 118 Braun L, Cohen M. Vitamin B6. Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:1088.
- 119 Natural Medicines. Vitamin B6. [Online]. 2016. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=934#scientificName. [Cited 16/01/17].
- 120 Braun L, Cohen M. Magnesium. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:677-692.
- 121 Braun L, Cohen M. Zinc. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2010:1197-1223.
- 122 Natural Medicines. Zinc. [Online]. 2017. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=982#scientificName. [Cited 16/01/17].
- 123 Natural Medicines. Magnesium. [Online]. 2016. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=998#scientificName. [Cited 16/01/17].
- 124 Natural Medicines. Glutamine. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=878. [Cited 16/01/17].
- 125 Braun L, Cohen M. Glutamine. In: Herbs and natural supplements; an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:631-643.
- 126 Natural Medicines. Magnesium. [Online]. 2016. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=998#scientificName. [Cited 16/01/17].
- 127 Braun L, Cohen M. Vitamin B3. Herbs and natural supplements: an evidence-based guide. 3rd ed. Sydney. Elsevier/Churchill Livingstone. 2010:936-945.
- 128 Natural Medicines. Vitamin B3. [Online]. 2016. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=924#scientificName. [Cited 16/01/17].
- 129 Natural Medicines. Iron. [Online]. 2015. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=1001#scientificName. [Cited 16/01/17].
- 130 Braun L, Cohen M. Vitamin C. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2015:979.
- 131 Natural Medicines. Taurine. [Online]. 2016. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=1024. [Cited 16/01/17].
- 132 Ehrlich SD. Gallbladder disease. University of Maryland Medical Center. [Online]. 2016. Available from: http://umm.edu/health/medical/altmed/condition/gallbladder-disease. [Cited 16/01/17].
- 133 Natural Medicines. Taurine. [Online]. 2016. Available from: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbssupplements/professional.aspx?productid=1024. [Cited 16/01/17].
- 134 Ehrlich SD. Vitamin B3 (Niacin). University of Maryland Medical Center. [Online]. 2015. Available from: http://umm.edu/health/medical/altmed/supplement/vitamin-b3-niacin. [Cited 16/01/17].
- 135 Braun L, Cohen M. Vitamin B3. In: Herbs and natural supplements: an evidence-based guide. 3rd ed. Sydney: Elsevier/Churchill Livingstone. 2010:942.
- 136 Braun L, Cohen M. Zinc. In: Herbs and natural supplements: an evidence-based guide. 4th ed. Vol 2. Sydney: Elsevier/Churchill Livingstone. 2010:1218.
- 137 Ehrlich SD. Possible Interactions with: Zinc. University of Maryland Medical Center. [Online]. 2007. Available from: http://umm.edu/health/medical/altmed/supplement-interaction/possible-interactions-with-zinc. [Cited 16/01/17].
Moderate Level Cautions
Theoretically, Glutamine, which is metabolised to the excitatory neurotransmitter glutamate, might antagonise the anticonvulsant effects of medications taken for epilepsy.110 Use with caution and monitor patient symptoms.
Vitamin B6 supplements may lower plasma levels and efficacy of these drugs. Monitor for drug effectiveness, and exercise caution when these drugs are being taken concurrently. High doses of pyridoxine should be avoided in people on these medications.111
Theoretically, glutamine, which is metabolised to the excitatory neurotransmitter glutamate, might antagonise the anticonvulsant effects of medications taken for epilepsy.112 Use with caution and monitor patient symptoms.
Pyridoxine at doses above 200 mg daily can reduce plasma levels of phenytoin. High doses of pyridoxine should be avoided in people on these medications.113
Use with caution in patients with known allergy/hypersensitivity to Monosodium Glutamate (MSG). Glutamine is metabolised to glutamate in the body and in theory may precipitate symptoms of MSG sensitivity. Use with caution and monitor patient symptoms, discontinuing use if allergic-type symptoms occur (e.g. redness, itchiness).114
Niacin and nicotinamide can cause histamine release. Supplementation may therefore exacerbate allergic symptoms in sensitive individuals. Use with caution in patients with known allergy/hypersensitivity to niacin or nicotinamide.115
