Metagenics Calcitite Osteo
Hydroxyapatite and Soy for Osteoporosis
Available in:
- Metagenics Calcitite Osteo Powder 234g
- Metagenics Calcitite Osteo 120tabs
- Metagenics Calcitite Osteo 60tabs
To support bone health:
Dosage: Take 2 tablets twice daily with food OR Add 1 scoop (3.9 g) to 200 mL of water twice daily with food. Stir well and take immediately.
A clinically effective combination of soy isoflavones, hydroxyapatite calcium, vitamin D and trace minerals to improve bone formation and density and slow the progression of osteoporosis.
Mechanism of Action/Clinical Research:
- Microcrystalline hydroxyapatite (MCHA) contains all the natural elements of healthy bone in a protein-mineral complex, providing calcium and phosphorus in the ideal 2:1 physiological ratio for bone mineralisation.[150]
In women with osteoporosis, MCHA providing 712 mg/d elemental calcium vs. 1000 mg/d of elemental calcium from calcium carbonate in addition to a vitamin D (266 µg/d) lowered the rate of bone mineral density (BMD) loss over three years more significantly in the MCHA group (p<0.05).[151]
- Glycine max (Soy Isoflav-One) extract is a non-genetically modified soybean extract containing a minimum of 40% isoflavones that act as SERMs through their phytoestrogenic actions.
Isoflavones have been shown to inhibit osteoclast proliferation and decrease bone resorption by osteoclasts.[152]
A meta-analysis including data from 1,240 menopausal women demonstrated ingestion of 82 mg/d of soy isoflavones for 6 to 12 months significantly increased spine BMD by an average of 2.38% (p<0.001) compared to controls.[153]
- 800 IU/d of vitamin D in combination with calcium may decrease the incidence of non-vertebral fractures by 10% to 20%, especially in persons in the older age groups with lower baseline vitamin D.[154]
- Boron plays a role in calcium balance through a number of different mechanisms, in particular, helping to reduce urinary calcium excretion and enhance calcium absorption.[155]
- Zinc may modulate the anabolic effect of insulin-like growth factor I (IGF-1) in osteoblasts, and may enhance the proliferative effect of oestrogen on these cells[156]
Osteoporosis
Calcium is the primary mineral required for skeletal strength,[1] a deficiency of which is associated with a decline in bone mineral density (BMD) [Figure 1].
The progressive decline of BMD weakens the bones, leading to osteopenia (defined as mild to moderate bone loss) and osteoporosis (defined as a severe bone loss)[2] and are associated with increased fracture risk, long-term morbidity and reduced quality of life.[3]
Further, women are at higher risk following a menopause-associated decline in oestrogen levels, which increases the rate of bone catabolism.[4],[5]
As such, a combination of highly-bioavailable microcrystalline hydroxyapatite calcium (MCHC) enriched with natural bone-growth factors, isoflavone-rich soy extract, and cofactors vitamin C, boron, zinc, manganese, vitamin K and vitamin D, offers an effective solution to mitigate calcium deficiency, reduce bone loss and support bone retention in individuals at risk of developing osteoporosis.[6]
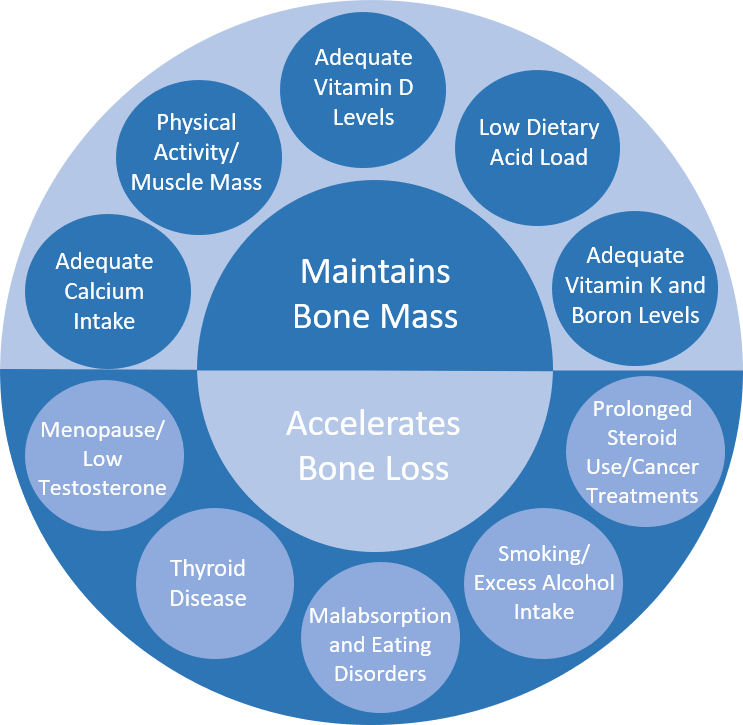
Figure 1: Health-related factors that influence an individual’s risk of developing osteopenia and osteoporosis.[7],[8],[9],[10],[11],[12],[13],[14],[15]
References
[1] Chandran M, Tay D, Mithal A. Supplemental calcium intake in the aging individual: implications on skeletal and cardiovascular health. Aging Clin Exp Res. 2019 Jun;31(6):765-781. doi: 10.1007/s40520-019-01150-5.
[2] The Royal Australian College of General Practitioners. Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age [Internet]. Melbourne, VIC: RACGP; c2016.; 2017 [cited 2020 Jun 9]. Available from: https://www.racgp.org.au/getattachment/2261965f-112a-47e3-b7f9-cecb9dc4fe9f/Osteoporosis-prevention-diagnosis-and-management-in-postmenopausal-women-and-men-over-50-years-of-age.aspx.
[3] Abimanyi-Ochom J, Watts JJ, Borgström F, Nicholson GC, Shore-Lorenti C, Stuart AL, et al. Changes in quality of life associated with fragility fractures: Australian arm of the international cost and utility related to osteoporotic fractures study (AusICUROS). Osteoporos Int. 2015 Jun;26(6):1781-90. doi: 10.1007/s00198-015-3088-z.
[4] The Royal Australian College of General Practitioners. Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age [Internet]. Melbourne, VIC: RACGP; c2016.; 2017 [cited 2020 Jun 9]. Available from: https://www.racgp.org.au/getattachment/2261965f-112a-47e3-b7f9-cecb9dc4fe9f/Osteoporosis-prevention-diagnosis-and-management-in-postmenopausal-women-and-men-over-50-years-of-age.aspx.
[5] Elsevier Clinical Key. Osteoporosis [Internet]. Melbourne (AUS): Elsevier; 2018 [updated Nov 7 2018; cited 2020 Jul 21]. Available from https://www.clinicalkey.com.au. subscription required to view.
[6] Health and Medical Research Council. Nutrient reference values for Australia and New Zealand. Calcium [Internet]. Canberra (ACT): Australian Government. 2017 September [cited 2020 Nov 3]. Available from: https://www.nrv.gov.au/nutrients/calcium.
[7] Elsevier Clinical Key. Osteoporosis [Internet]. Melbourne (AUS): Elsevier; 2018 [updated Nov 7 2018; cited 2020 Jul 21]. Available from https://www.clinicalkey.com.au. subscription required to view.
[8] Elsevier Clinical Key. Osteoporosis [Internet]. Melbourne (AUS): Elsevier; 2018 [updated Nov 7 2018; cited 2020 Jul 21]. Available from https://www.clinicalkey.com.au. subscription required to view.
[9] Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, et al. The National Osteoporosis Foundation's position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int. 2016 Apr;27(4):1281-1386. doi: 10.1007/s00198-015-3440-3.
[10] The Royal Australian College of General Practitioners. Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age [Internet]. Melbourne, VIC: RACGP; c2016.; 2017 [cited 2020 Jun 9]. Available from: https://www.racgp.org.au/getattachment/2261965f-112a-47e3-b7f9-cecb9dc4fe9f/Osteoporosis-prevention-diagnosis-and-management-in-postmenopausal-women-and-men-over-50-years-of-age.aspx.
[11] Elsevier Clinical Key. Osteoporosis [Internet]. Melbourne (AUS): Elsevier; 2018 [updated Nov 7 2018; cited 2020 Jul 21]. Available from https://www.clinicalkey.com.au. subscription required to view.
[12] Elsevier Clinical Key. Osteoporosis [Internet]. Melbourne (AUS): Elsevier; 2018 [updated Nov 7 2018; cited 2020 Jul 21]. Available from https://www.clinicalkey.com.au. subscription required to view.
[13] Wong PK, Christie JJ, Wark JD. The effects of smoking on bone health. Clin Sci (Lond). 2007 Sep;113(5):233-41. doi: 10.1042/CS20060173.
[14] Kogawa M, Wada S. Osteoporosis and alcohol intake. Clin Calcium. 2005 Jan;15(1):102-5. PMID: 15632479.
[15] Wynn E, Lanham-New SA, Krieg MA, Whittamore DR, Burckhardt P. Low estimates of dietary acid load are positively associated with bone ultrasound in women older than 75 years of age with a lifetime fracture. J Nutr. 2008 Jul;138(7):1349-54. doi: 10.1093/jn/138.7.1349.
Metagenics Calcitite Osteo
Metagenics Calcitite Osteo 120tabs
Metagenics Naturopathic Medicines
Metagenics Calcitite Osteo 60tabs
Metagenics Naturopathic Medicines
Metagenics Calcitite Osteo Powder 234g
Metagenics Naturopathic Medicines